DIRECTIONS FOR FURTHER SPATIAL RESEARCH ON COVID-19
(Source: Newsletter 2/2020 | Arbeitskreis Medizinische Geographie und Geographische Gesundheitsforschung in der Deutschen Gesellschaft fur Geographie)
During the last months, like probably many of us working in GeoHealth, I felt like living my own research. Given that normally my work and private life are strictly separated, this is a very unusual experience. Since the beginning of the Covid-19 pandemic, my work on modelling of infectious diseases (Abdulkareem et al., 2020; Abdulkareem et al., 2019) has taken some unexpected turns, sometimes strengthening the paths I was already following (implementing risk perception in agent-based models), but also giving my research new turns. The following points are some of the issues I was confronted with:
Risk perception
Over the past years, I have implemented risk perception into agent-based simulation models. This modelling was mainly done on cholera, yet the underlying principles are equally important for Covid-19. When we want to simulate the spread of an infectious disease realistically, we need to take into account the way people respond to this disease. Modelling the human response asks for models that integrate disease spread and human decisions. These models require data about risk perception and coping appraisal, as the perception of risk will trigger a response (change of behaviour) which might affect the chance of infection. There are many dimensions of the inclusion of risk perception that are yet unexplored like risk perception per age category or geographic region. During the ongoing Covid-19 pandemic, we have seen that representatives of different age groups perceive different levels of risk. Younger people experience milder symptoms and will judge the severity of the disease differently from their parents or grandparents. We also observed that different countries choose different types of coping strategies. While some countries accepted face masks as a good preventive measure and coping strategy from the early phases of the epidemic, The Netherlands, for example, only recently adopted this coping behaviour. This pandemic showed us that a lot more work is needed on modelling approached that combine disease diffusion and human behaviour.
Spatial patterns
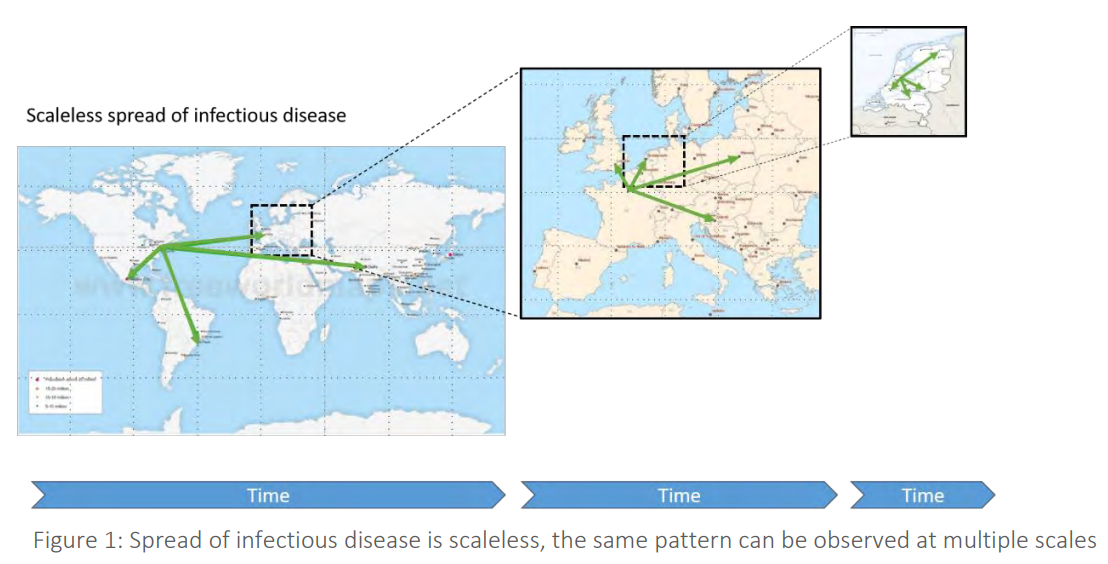
Many maps of Covid-19 were produced over the past months (e.g. for the Netherlands by RIVM), and many dashboards were published to visualize and follow the disease spread (e.g. by Johns Hopkins University). For me, this is not the same as trying to understand disease diffusion patterns. Maps and dashboards alike are very helpful to evaluate the difference in the number of disease cases in space and time, but other questions remain unanswered. I always tell the students I teach that disease spread is scaleless, like a fractal. We expect that the disease will spread like the popularity of a new electronic device (from early adopters to the large majority) and like the popularity of a pop group, from local to global. Disease spread is triggered by human movement. The spatial patterns we see will show the infection move up the urban hierarchy to a very large city, followed by a downward cascading spread. From a large city to other large cities based on our air travel flight patterns, from each of these cities to smaller towns in the vicinity (local air travel or long-distance trains), and from these smaller towns to villages due to daily commuting. Besides these hierarchies, infectious diseases can become endemic in areas where the population is large enough. The threshold population needed for this is often defined as the Critical Community Size (CCS) a concept which I extended in the past to a Critical Community Region (CCR) (Augustijn, 2018), a spatial zone that we can delineate where the disease maintains itself and that acts as the source of further spread. An area that seems to be hardly touched in this Covid-19 crisis would detect these types of spatial patterns. Can we find hierarchies in the disease spread and do we notice and can we delineate CCRs? This information may not facilitate an immediate end to Covid-19, but we may gain knowledge that might be helpful for future disease outbreaks.
The Global South
At the beginning of the Covid-19 pandemic, we were approached to develop Covid-19 models for other countries, explicitly for Afghanistan and Iraq. Although we already had an agent-based Covid-19 model for the Netherlands, we realized (again) that converting this model to serve another country is very difficult, for two reasons: The lack of necessary input data (e. g. detailed commuting data, detailed population data), and the local knowledge needed for such a conversion. These are not problems easily solved, but sharing our expertise in model development and data collection can help. For a disease like Covid-19, we need the combined efforts of all countries around the globe to combat the disease and win the fight.


